Introduction: Acquired hemophilia A (AHA) is a rare bleeding disorder characterized by autoantibodies against factor VIII (FVIII). Delayed diagnosis is frequent, resulting in morbidity and health resource utilization. Predictors of diagnostic delays and their impact on outcomes are unclear.
Aims: 1) Evaluate the time from presentation to AHA diagnosis, in a large Canadian province, 2) examine predictors of diagnostic delays, and 3) assess the impact of delays on outcomes and resource utilization.
Methods: This multicentre retrospective cohort study included adults (≥18 years) diagnosed with AHA (January 2000-December 2021) in Alberta, Canada. Alberta's 661,848 km 2 geographic area encompasses two adult hemophilia treatment centres (HTCs). We assessed the prevalence of delayed diagnosis (from bleeding or first prolonged aPTT) and examined the impact of sociodemographic variables (age, sex, rural residence, living arrangement, initial presentation to HTC) and disease variables (AHA etiology, major bleed at presentation, comorbidities, FVIII activity and inhibitor titre) on the diagnostic delays. Case-based analysis and logistic regression were used to identify contributory factors and predictors of diagnostic delays, respectively. Kaplan-Meier curves were used to estimate overall survival (OS), and Cox proportional hazards regression analysis was used to assess the impact of diagnostic delays on OS. Ethics board approval was obtained.
Results: Of the 38 patients diagnosed with AHA, 25 (66%) were female, 8 (21%) resided in rural areas, and 10 (26%) resided >100 km from HTC. Median age was 74 years (IQR 61-81), with marked comorbidities (median Charlson comorbidity index [CCI] 5, IQR 3-7). Most patients (27; 71%) initially presented to non-HTCs while 32 (84%) were eventually admitted to HTCs. At presentation, 27 (71%) had ISTH major bleeding and 13 (34%) were on anticoagulants or antiplatelets/NSAIDs.
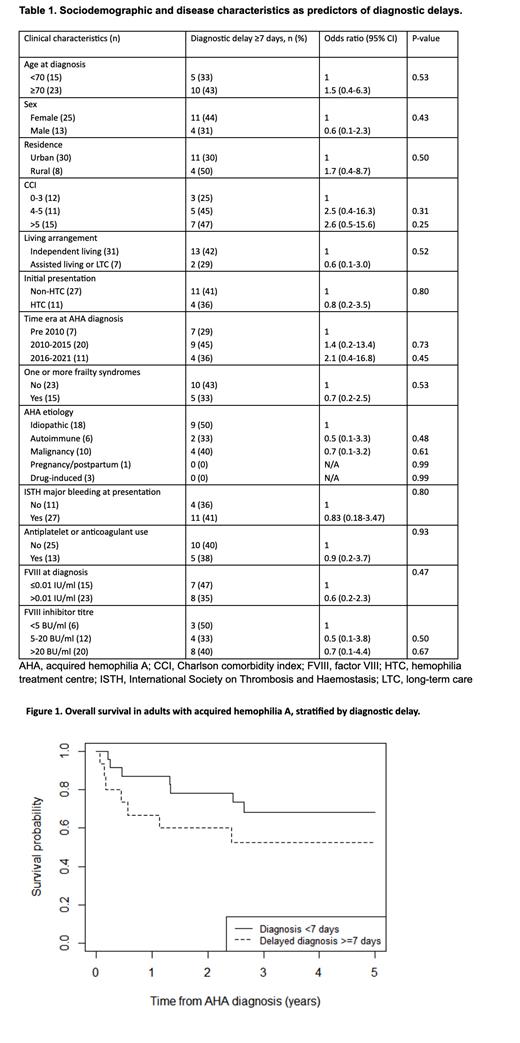
The median time from bleeding symptom and prolonged aPTT to diagnosis was 3.5 days (IQR 0-11.0) and 3.5 days (IQR 1.3-9.5), respectively. From first bleeding symptom, diagnosis was delayed ≥7 days in 15 (39%) patients and >30 days in 2 (5%). Case-based analysis identified the top reasons for delays ≥7 days: delayed ordering of aPTT from 7-62 days after bleeding (6/15; 40%), delayed ordering of mixing study following first abnormal aPTT from 7 days to >1 year (9/15; 60%) and attribution of bleeding to antiplatelets/anticoagulants (5/15; 33%). Neither demographic nor disease characteristics were identified as significant predictors of delayed diagnosis by logistic regression (Table 1). Initial presentation to HTCs had no impact on time to diagnosis. While non-statistically significant, there appears to be a clinically significant temporal gradient suggesting higher odds of diagnostic delays in 2010-2015 (OR 1.4) and 2016-2021 (OR 2.1) compared to pre-2010.
Delayed diagnosis was not significantly associated with hospitalization rates, LOS, bypassing agent consumption, or units of packed red cells or plasma transfused. At a median follow-up of 3 years, 18 patients (47%) died at a median of 7 months (IQR 3-30). The most common causes of death included: infection (4), malignancy (3), bleeding (2), and thrombosis (2). Delayed diagnosis ≥7 days was associated with a non-significant trend towards worse 3-month OS (80% vs 91%) and 1-year OS (67% vs 87%, log-rank P=0.40; Figure 1). On Cox proportional hazards analysis, male sex (HR 4.0, 95% CI 1.5-10.5) and CCI 4-5 vs 0-3 (HR 7.0, 95% CI 1.5-32.3), but not delayed diagnosis (HR 1.5, 95% CI 0.6-3.9) were associated with increased hazard of death.
Conclusion: In our large geographic catchment area, in the absence of an AHA reference centre, the median time to diagnosis (3.5 days) was markedly shorter than that reported in other single-centre studies (14-19 days), although delayed diagnosis ≥7 days was common. We did not identify statistically significant predictors of diagnostic delays, likely limited by small numbers. However, case-based analysis highlighted knowledge gaps as contributory factors, such as delayed ordering of aPTT in bleeding patients and delayed mixing study if aPTT is prolonged. Interestingly, time to diagnosis did not improve in recent years or with initial presentation to HTCs. Given the potential impact of delays on morbidity/mortality, further education is needed to expedite diagnosis in both HTCs and community settings.
Disclosures
Goodyear:Sanofi: Honoraria; Alexion: Honoraria; Pfizer: Honoraria; Sobi: Honoraria; Takeda: Honoraria; Medison: Honoraria; Roche: Honoraria; BioCryst Pharmaceuticals: Honoraria; CSL Behring: Honoraria. Sun:Takeda: Honoraria; Sobi: Honoraria; Sanofi: Honoraria; Pfizer: Honoraria; Shire: Honoraria.